Pulmonary RRP
While rare, in more aggressive cases, RRP can migrate down the airway and into a patient’s lungs. It may stay benign or it may become malignant. There is currently no cure, though we are working hard to change that.

Pulmonary Spread of RRP
While rare, pulmonary spread of Recurrent Respiratory Papillomatosis can and does occur. Several recent papers published on this rare complication of RRP have shown that 12-15% of RRP patients will have distal spread (disease on the trachea, carina, bronchus) and 7-9% of RRP patients will have pulmonary spread into the lungs.
Pulmonary spread of RRP is often found incidentally (found while looking for another medical issue unrelated to RRP) or found when a RRP patient presents with shortness of breath, coughing up blood, or when a cough has lingered and does not respond to treatment. The gold standard for locating pulmonary RRP is by CT scan, as a lung x-ray typically will not show pulmonary RRP in its earliest stages (when the nodules are smaller).
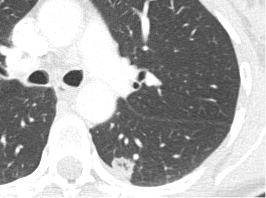
An Image of Pulmonary Spread of RRP
In this CT image is a 2.5CM lung nodule (lower lobe) that is biopsy confirmed to be squamous cell papillomatosis, HPV 11. This patient is a JORRP who is now an adult. Pulmonary RRP should be treated at expert centers who have had previous pulmonary patients.
Are there risk factors for pulmonary RRP?
The RRPF reports from the RRP Patient Registry/CoRDS that tracheal disease, aggressive JORRP disease, and/or prior or current tracheostomy are common responses by those patients with pulmonary disease. Age of diagnosis is also believed to play a role in risk of pulmonary spread. The RRPF is working towards a screening protocol being the standard of care for those patients clinicians deem at risk.
How is pulmonary spread of RRP confirmed?

Pulmonary spread of RRP is often first suspected after a bronchoscopy or CT scan of the lungs. It is confirmed by biopsy.
What does the disease do once in the lung space?
Pulmonary spread of RRP often cavitates, which can occur in multiple lobes. A lung cavity is defined radiographically as a lucent area contained within a consolidation, mass, or nodule. This is not a metastasis when in multiple areas, but rather individual processes. Pulmonary spread of RRP can become infected, causing repeated respiratory infections, or pneumonias. Generally, the pulmonary spread of RRP is asymptomatic. However, any new cough that does not resolve or coughing up of blood or bloody mucus, or shortness of breath that does not resolve after a RRP surgery, should be further evaluated by your care team. The nodules can grow, most often slowly, and they can become malignant. It is important for any pulmonary spread to be monitored for changes. Pulmonary spread of RRP, even if benign, can create life-threatening complications.
Are there any treatments for pulmonary spread of RRP?
There are no FDA approved pharmaceutical treatments for pulmonary spread of RRP. Surgical treatment (wedge resection, lobe removal, EBUS) is sometimes the method recommended if the papilloma has blocked an airway or is exhibiting changes that are concerning for malignancy. Other methods used include Radio Frequency Ablation, off-label drug therapies such as Bevacizumab (Avastin), checkpoint inhibitors (PDL1+) such as Keytruda, as well as other oncologic drugs based upon lab results as to what the patient would respond to. None of these treatments are curative of pulmonary spread of RRP. The RRPF works with patients dealing with pulmonary spread to help guide them in this complication of RRP and will facilitate this upon contact by the pulmonary patient.
If you have the pulmonary disease removed by surgery, does it come back?
Unfortunately, the pulmonary spread of RRP can and often does return after removal of a nodule. One theory is that surgery can further seed the virus to other areas. Discuss the pros and cons of removal with your care team.
Does pulmonary spread of RRP become cancerous?
While rare, pulmonary spread of RRP can become cancerous and tends to respond poorly to current squamous cell carcinoma treatments. We are working with researchers to better determine why the poor response occurs and possible treatments that would create a better response.
What is the treatment option once the pulmonary disease becomes cancer?
Once the disease has become malignant, surgical removal, interventional pulmonary methods and/or use of oncology drugs are then added to your care plan if they are not already in place. The biopsy result will read “squamous cell carcinoma arising from respiratory papillomatosis.”
Does Pulmonary Spread Happen in Adults and Children?
Pulmonary spread most often takes place in those who were diagnosed as JORRP, but it can also occur in AORRP patients. Unfortunately, the RRPF has seen pulmonary spread in infants, very young children, teenagers, young adults and older adults.
Who should be part of a pulmonary patient care team?
Most pulmonary patients are followed by their RRP ENT, an interventional pulmonologist, as well as an oncologist if the patient is on any pharmaceutical therapy. If a surgeon is needed, a thoracic surgeon may be added to the team. The RRP ENT typically leads the team, as they are the most experienced with the disease.
Who are centers/clinicians who have had prior pulmonary RRP patients?
The RRPF hopes to identify Pulmonary Centers of Excellence soon, but we can provide a database of clinicians that have seen patients with pulmonary spread of RRP. To access this database, click here. It is important to note that there is no true expert for the treatment of pulmonary spread of RRP, but being with a clinician who has had prior or current patients with this complication can offer a better outcome than choosing to stay with a care team with no prior experience. The RRPF encourages all pulmonary patients to reach out to the RRPF so that we can help you in this journey.